February 17, 2021
My emergency department colleagues and I are in year two of a dual pandemic. The devastating social, emotional and economic effects of COVID-19 are exacerbating the scale of what was an already out-of-control opioid use disorder crisis that is playing out in emergency departments like mine across the country. More than 40 states reported increases in opioid-related mortality in 2020, and that stacks up with what my colleagues and I are experiencing in our Philadelphia emergency department.
As an emergency physician, treating opioid use disorder (OUD) can be
physically grueling. I’ve been attacked and spit on, and one patient
(actively and uncontrollably withdrawing from heroin) flooded our emergency
department by clogging the sinks with sheets and physically sat in the sink
like an agitated and scared bird, trying to cool her fully aroused skin. It
can be emotionally debilitating for our patients, their families, and for
our providers.
"The faces of the patients — teens, young adults, seniors, parents, and friends — I’ve worked to resuscitate after an overdose haunt me. Many survive. Some don’t."
I remember a young man in his twenties who was found unconscious on the street in South Philadelphia. He had been injecting heroin and still had a homemade tourniquet on his arm when he was brought into the ER. He was cold and his heart had stopped. First responders gave him CPR en route to the hospital and my team and I got his heart beating again. We sent him to the ICU to recover. He died on Mother's Day without ever regaining consciousness or saying goodbye to his family.
I also remember another patient who was unresponsive when he was brought in by his distraught brother after they ingested an unknown powder several hours prior. His brother, still intoxicated himself, was at his bedside in the ICU when he died.
My fellow ER doctors have so many stories like this. I am frequently left wishing I could do more or that the patient had come to my emergency department earlier. But what often leaves me crying at night is the knowledge that cumbersome treatment barriers and outdated stigma keep patients from getting the care they need.
Stigma costs lives. Stigma can kill.
And stigma doesn’t just come from your next-door neighbor judging your
husband or daughter with OUD, stigma is pervasive in the medical field as
well.
OUD treatment needs to be comprehensive, but access to care can start in
the ED. But one of the best tools we have to offer — Suboxone and its
generic buprenorphine/naloxone which is prescribed for the treatment of
opioid dependence — is out of reach for many patients and providers because
of outmoded prescribing restrictions. Buprenorphine is effective, safe, and
reduces opioid cravings as well as withdrawal symptoms. In order to
prescribe buprenorphine, physicians are required to have an “X-waiver,” a
requirement that takes many hours, as well as Drug Enforcement
Administration (DEA) registration and ongoing compliance.
I am X-waivered, and have seen how Suboxone can lead to patient success: a road to sobriety, a life off the streets, and a place back in society with family and true friends. But the requirement can lead to misconceptions and stigma about medication-assisted treatment and other clinicians are unwilling to pursue an X-waiver, leading to less providers and less access to treatment options for patients. Only 2.2% of physicians in America have an X-waiver and most of us, 90.4%, practice in urban areas leaving many in suburbs and rural areas without access to buprenorphine treatment as an option.
There were more than
81,000 drug overdose deaths
in the United States in the 12 months ending in May 2020, the highest
number of overdose deaths ever recorded in a 12-month period. And in
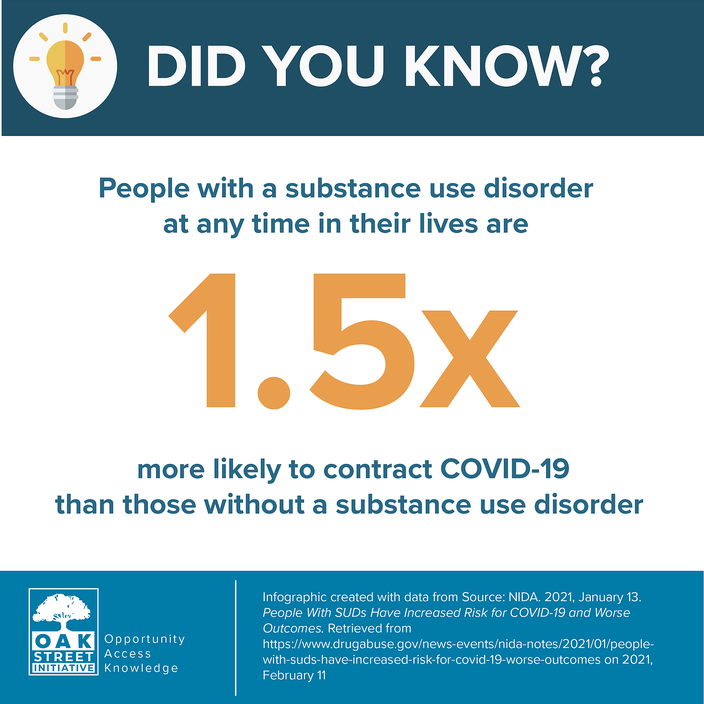
certain parts of the country, drug overdose deaths outpaced COVID deaths. Those with a substance use
disorder are
at increased risk for contracting COVID-19
and have worse outcomes than those without substance abuse disorders. With
increased attention rightly focused on tackling COVID, immediate action is
needed to tackle the opioid epidemic as well.
Many emergency physicians like myself hoped a recent change in guidelines could prove to be a game changer. This January, the U.S. Department of Health and Human Services effectively removed the X-waiver for physicians registered with the DEA who treat no more than 30 patients with buprenorphine. For emergency medicine physicians like myself, the patient limits did not apply to the January rule change as so many with OUD seek access to care though the emergency department. However, despite praise from the American Medical Association and physicians like me, the X-waiver rule change was shelved within weeks of its announcement due to legal concerns over implementation.
Like many illnesses, there is no one cure for OUD, but changing the X-waiver would be a major step, and it is one that will save lives. And in this duel pandemic where my colleagues and I have seen too much death and are surrounded by too much sadness, we need a change that will allow us to provide care to more patients in a compassionate, comprehensive way.
Opinions expressed in this article do not represent those of the University of Pennsylvania Health System or the Perelman School of Medicine.