After living through two years of the COVID-19 pandemic, we’ve all learned that the situation can rapidly change. Public health guidelines continue to constantly evolve at the national, state, and local level as new information about cases and variants becomes available.
But regardless of the current trends and case numbers, we all still face a daily risk of being exposed to the virus. Here’s a simple guide on how to take care of the people around you and protect your health if you have been exposed to someone with COVID-19, have symptoms, or test positive.
When to Test Yourself for COVID-19
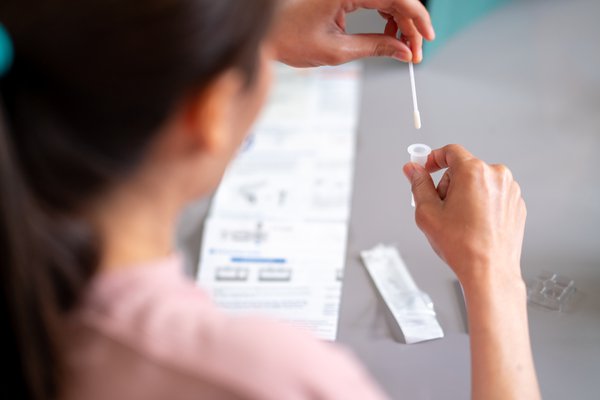
At-home COVID-19 tests use a swab of cells taken from your nose or throat to look for certain proteins indicating active COVID-19 infection. Results are usually seen in 10 – 20 minutes.
This fast turnaround, and the fact that these tests can be taken anytime and anywhere, make them a very important resource for saving lives and preventing spread.
You can now find at-home tests in many pharmacies. Take-home tests are available for free at many vaccine clinics, and you can order them at no cost from the federal government. Independence Blue Cross (Independence) also covers up to 8 over-the-counter (OTC), FDA-approved tests per calendar month as required by the Biden Administration.
Here are the best situations and times to test yourself:
• If you have any COVID-19 symptoms, you should take an at-home test immediately.
• If you’ve been exposed to COVID-19, you should wait at least five days to test yourself. If you do it any earlier, you could still be infected even if you get a negative result. If you do test negative, consider testing yourself again 1 – 2 days after your first test.
• If you’re planning to attend an indoor event or gathering — especially around people at high risk of severe disease, older adults, those who are immunocompromised, or people who haven’t been vaccinated — it’s best to test yourself immediately before the gathering or as close to the beginning of the event as you can.
These recommendations, like many other things about COVID-19, change frequently. So check the CDC’s guidelines to make sure they’re still current.
But what if you’ve been exposed, have tested positive, or are sick with COVID-19? According to the CDC:
If you’ve been exposed, you should quarantine for at least 5 days. If you’ve had a booster shot, you don’t need to quarantine, but you should wear a mask for 10 days. This means staying away from others outside your home.
When to Isolate
If you are sick, or have tested positive for COVID-19, you should isolate for at least 5 days. This means avoiding contact with others, even the people you live with. It’s best to stay in a specific “sick room” or area of your house, and use a separate bathroom if one is available.
When to Seek Treatment
Most people infected with COVID-19 have only mild symptoms (like fever, cough, headache, or muscle pain), or might not have any symptoms at all. This is especially true for those who have been fully vaccinated and have received their booster. It’s also especially true for the Omicron variant.
If you have only minor or no symptoms, you will probably not need any medical consultation or care. And with the extreme stress that the pandemic has placed on our health care system, it’s best to avoid adding to that burden if you don’t have to.
But if you’re concerned about your symptoms or your risk of severe disease, make an appointment with your primary care doctor to discuss your treatment options.
For high-risk patients, treatment to prevent worsening of COVID-19 symptoms is now available in the form of a pill. This FDA approved medication is called, Paxlovid (also known as nirmatrelvir tablets; ritonavir tablets), and is available by prescription to high-risk patients, who are not admitted to the hospital. Speak to your doctor to see if this pill is right for you.
You may qualify for Paxlovid if you are:
• Within 5 days of experiencing mild to moderate COVID-19 symptoms
• Confirmed to be COVID-19 positive via PCR or rapid antigen test
• Considered high risk for complications related to COVID-19 infection
Whether you have received Paxlovid or not, do seek emergency medical care if you have:
• Trouble breathing
• Persistent pain or pressure in your chest
• Inability to wake up or stay awake
• Inability to drink fluids
• Pale, gray, or blue-colored skin, lips, or nail beds (depending on your skin tone)
The Best Ways to Protect Yourself and Your Loved Ones
I can’t say this often or emphatically enough: If you haven’t been vaccinated against COVID-19, please do it now. If you’ve been vaccinated but haven’t gotten your booster, please do that now. If other people in your home aren’t vaccinated and/or boosted, please encourage them to take care of this.
According to the CDC, people who are unvaccinated are 21 times more likely to die from a COVID-19 infection than those who have received a primary vaccination series and a booster. The next life the vaccines save could be your own. Or the life of one of your parents. Or the life a friend who’s immunocompromised and can’t benefit from the protection of the vaccine.
We don’t know what the future holds. But as long as COVID-19 keeps spreading, some health precautions will be needed and dangerous new variants could evolve. So to help bring this pandemic to an end, please get vaccinated, keep getting boosters as recommended, and follow responsible precautions — like wearing a mask in appropriate situations.
This content was originally published on IBX Insights.
About Dr. Dolores Roman
Dr. Dolores Roman joined Independence Blue Cross in 2019. As a 20-year veteran of emergency rooms in and around the Philadelphia area, Dr. Roman has dealt with every kind of emergency. Now as a medical director at Independence, Dr. Roman is involved in utilization management, case management, and quality improvement. What Dr. Roman loves most about this job is the opportunity to collaborate with colleagues in order to enhance the health and well-being of those served by Independence Blue Cross.