
March 20, 2020
 Source/Image licensed from Ingram Image
Source/Image licensed from Ingram Image
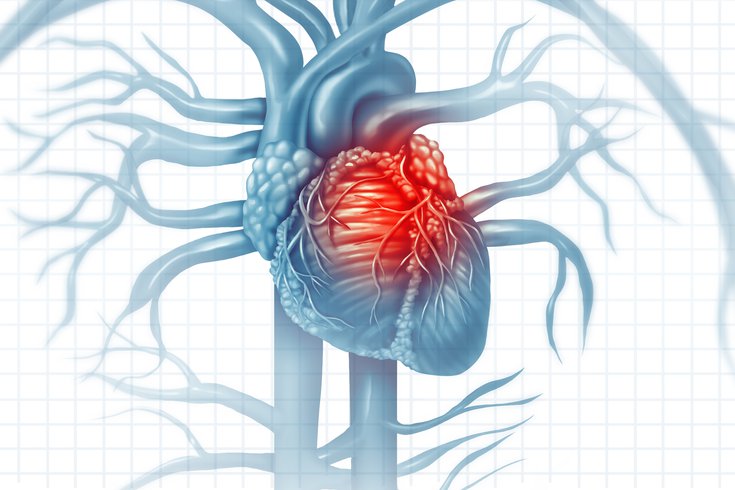
People with heart disease appear to be at higher risk of developing severe cases of COVID-19. A coronavirus infection attacks the lungs, causing the heart to work much harder in its efforts to distribute oxygen throughout the body.
The novel coronavirus has taken the world by storm. Three months ago, it was relatively unheard of, and now it dominates the headlines. As such, it has provoked a lot of anxiety.
Coronaviruses were first discovered in the 1960s, when they were identified as being responsible for relatively benign upper respiratory infections in children and infants. Many coronavirus variations, or strains, have emerged over the past several decades including one that caused SARS, a rapidly aggressive severe acute respiratory syndrome.
SARS originated in Southern China before rapidly spreading throughout the world in 2002-2003. It left death and destruction in its path, but not to the extent that is presently being observed with this new strain of coronavirus, known as SARS-CoV-2.
Despite the fact that coronaviruses have been around so long, there is still so much we don’t know, particularly when it comes to the current strain. What we do know is the following.
The average age of individuals who have died from COVID-19, the disease caused by the current strain, is 70 years and the majority of these patients had underlying health problems, including heart disease. That prompted the U.S. Centers for Disease Control and Prevention’s warning that adults older than 60 years should take special precaution.
In the early studies from China, death was more likely to occur in individuals with diabetes or heart disease. This does not necessary mean that individuals with heart disease are more susceptible to the coronavirus, but rather are more likely to have a worse outcome if they become infected. The good news for healthy, younger people is that for them, the coronavirus usually only causes mild, cold-like symptoms.
The main target of the virus is the lungs, resulting in pneumonia and leading to difficulty in oxygen getting into the blood to be delivered to all the vital organs. In this type of situation, the heart has to work that much harder, putting a stress on the heart. That is true for both normal functioning hearts, but even more so for patients with heart dysfunction and heart failure. Studies of previous coronaviruses, such as the one that caused SARS, have provided insight into the problems that potentially can be caused by COVID-19, including inflammation of the heart muscle, heart attacks and heart failure.
Dr. David Fischman, top, and Dr. Michael Savage.
As we age, our immune systems become weakened, which may be truer for individuals with heart disease. A weakened immune system may be responsible for an increased and prolonged inflammation resulting in damage to the heart and other organs, and partially responsible for the worse outcomes in these patients.
In patients with already present heart disease, further stress on the heart can be taxing and cause for the recommendation that individuals with heart disease limit their potential exposure to the virus. Many patients with heart disease have coexisting diabetes, which also has an effect of weakening the immune system. That makes them even more susceptible to worse outcomes.
Does COVID-19 pose any more risk to the heart patient than the flu virus, which according to the CDC had resulted in more than 16,000 deaths in the United States thru mid-February? The belief is that the risk may be higher than the flu as it has the ability to spread much easier, potentially resulting in more than the 29 million cases of flu that have occurred this season and ultimately more deaths.
With the flu season, there is more certainty as to its seasonal time course and expected outcomes. With the novel coronavirus, it is the uncertainty that is problematic. We still don’t know how many patients are truly infected. A contributing factor leading to the spread of this disease is the latent period between transmission and development of symptoms. A new study from Johns Hopkins estimates that it takes on average 5.1 days for symptoms to appear after a person gets infected.
As with the recommendations with the flu, it is imperative that we are particularly diligent in doing all we can to prevent the spread of this virus. This includes washing hands, keeping surfaces clean and avoiding travel to or being in places that may increase the risk of exposure.
This is particularly true for the heart patient. Does it mean that the patient with heart disease needs to avoid the gym? No, but with most gyms closing due to the need for social distancing, this has become a moot question.
Exercise is a good stress reliever particularly in stressful times such as this. It is also good for the immune system. So, with the gym closed, there are plenty of opportunities to exercise, including walking outdoors. Many gyms, including Jefferson’s Kennedy Fitness, offer in home-workouts which are live-streamed via Facebook and other internet sources. With the potential for stricter quarantine or shelter-in-place directives, this would be a great way to spend one’s time at home with clear health benefits.
Lastly, just as the virus has become rampant and now officially labeled a pandemic by the World Health Organization, so has the misinformation about the virus. Social media is not the best place to find updates. Rather, one should focus on reliable sources, including the CDC and WHO, whose job it is to protect us. In the meantime, wash your hands, clean surfaces and distance yourself to stay healthy.
 Jefferson Health/.
Jefferson Health/.