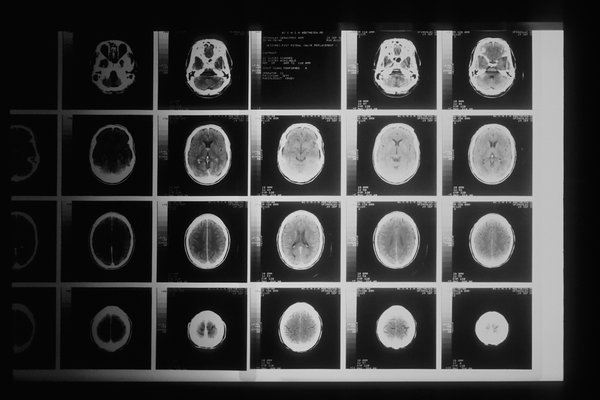
During the early phase of the COVID-19 pandemic, when hospitals were overwhelmed and people were avoiding going to the doctor's office, delays in computer tomography scans for cancer were expected.
However, a new study points to the alarming fact that many people who need imaging to detect and treat cancers are still not getting it, raising concerns of more advanced cancers and worse outcomes.
- MORE HEALTH
- Alcoholism drug has potential as a COVID-19 treatment, but studies are just getting underway
- Stillbirths are more prevalent since the delta variant emerged, CDC study finds
- Brandywine, Jennersville hospitals to remain open after Tower Health finds new ownership
In the study, researchers compared cancer-related CT exams during three periods of 2020: the pre-COVID phase from January to mid-March, peak COVID between mid-March to May and post-COVID from May to mid-November.
They found that CT for cancer screening dropped 82% during the peak of the pandemic. CT for initial workup, tracking active cancer and cancer surveillance also significantly declined.
Compared with pre-COVID numbers, volumes for cancer screening and initial workups have not fully recovered, with the numbers remaining down by 11.7% and 20%, respectively.
Interestingly, the drop in CT volumes occurred more in outpatient departments, while the number of imaging occurring in emergency departments increased after the peak period.
"The decline during the COVID peak was expected because of stay-at-home orders and the number of imaging departments that shut down as a precaution," said Dr. Marc Succi, an emergency radiologist at Massachusetts General Hospital. "Once normal operations resumed, you'd expect that these patients were being imaged in an equitable way, but, in fact, it turns out that they weren't."
Fear of contracting COVID-19 at the hospital or the doctor's office appears to continue to be a big driver of delays in routine health care, including CT imaging.
Another factor is that the pandemic isn't over, and some hospitals in COVID-19 hotspots are still rationing services so they can handle influxes of patients.
Succi said these delays in routine imaging and follow-up appointments will likely increase advanced cancers and cancer deaths.
"When initial diagnostic imaging is done in the emergency room, that suggests that people were having symptoms due to cancer for months and months, and they weren't checking in with their primary care providers," added Ottavia Zattra, a fourth-year medical student at Harvard Medical School. "Ultimately, the symptoms got so bad they couldn't handle it at home."
Concerns over delays in life-saving diagnoses and treatments have been raised since early in the pandemic. A Quest Diagnosis analysis conducted in 2020 found that the average weekly number of newly diagnosed cancer patients fell by an astounding 46.4% among the six most common types. They include breast, colorectal, lung, gastric, pancreatic and esophageal cancers.
The biggest decline was in breast cancer diagnoses, which fell by 51.8%. Pancreatic cancer diagnoses fell the least, at 24.7%. The drop-offs occurred in both routine screenings and diagnostic tests ordered in response to concerning symptoms.
Similar trends have been reported by the electronic medical records vendor Epic and the COVID and Cancer Research Network. Epic also found that even after screenings had picked up again, the numbers were still lower than they were before the pandemic.
These continued delays in routine care has oncologists worried because the earlier the diagnosis and treatment, the better the outcomes for cancer patients. The National Cancer Institute has projected 10,000 additional deaths in the United States due to breast and colorectal cancers alone over the next 10 years because of pandemic-related delays in diagnosis and treatment.
Rationing care across the board
It is not just cancer care that has been impacted by the continuing COVID-19 pandemic. According to a recent poll from NPR, the Robert Wood Johnson Foundation and the Harvard T.H. Chan School of Public Health, almost 1 in 5 American households have had to delay care for serious illness just in the past few months.
In states that have been hit particularly hard by the delta variant, like Idaho, some hospitals have had to ration care, telling patients they have to wait for surgery even when they have a serious condition.
Dr. Dan Zuckerman, medical director for St. Luke's Cancer Institute, told NPR that his staff has had to delay surgery for some breast cancers, initially treating them with hormones first.
The researchers of the CT imaging study, who are presenting next week at the annual meeting of the Radiological Society of North America, say that there needs to be more outreach to ensure that patients know they should still make their CT imaging appointments and other routine care despite COVID-19. Hospitals have multiple layers of protection in place to keep their patients and staff safe.
They also suggested that more resources should be diverted to community centers which may be handling a larger influx of patients still wanting to avoid larger academic hospitals. They also called for 24/7 imaging in emergency departments.
Succi and colleagues are planning to continue to track CT imaging volumes through 2021 and study whether race, language and income also affected access to cancer imaging during the pandemic.